COMPREHENSIVE OVERACTIVE BLADDER CENTER & INTERSTIM CENTER OF EXCELLENCE
Bladder control problems affect tens of millions of people every day. Do you go more than 8 times per day? Are you urinating often or frequently (i.e., peeing a lot), feeling like you have to pee a lot or have a strong sudden urge to urinate, leaking poop or have bowel incontinence, asking yourself “why do I have to pee so much” or “why am I peeing so much?”, or you’ve tried bladder control medicine and can’t tolerate the side-effects or they are no longer effective? If so, WE CAN HELP. We’ll identify the root cause of your bladder problem to provide the best treatment for overactive bladder. Enjoy a pleasant, anxiety and pain-free experience. We know how to cure overactive bladder and improve your quality of life.
COME TO THE BEST IN THE WORLD FOR OAB TREATMENT
We are the first Medtronic Overactive Bladder Center of Excellence in the world because of our amazing overactive bladder solutions and great outcomes. Schedule an appointment now to improve your quality of life.
6 REASONS TO COME TO ADVANCED
FACTS ABOUT OAB
THE ADVANCED JOURNEY TO SUCCESS
LIFESTYLE CHANGES
Lifestyle changes include diet, fluid, stress, sleep, exercise modification and weight loss. When lifestyle changes don’t help in a meaningful way, it’s time to consider medications.
MEDICATIONS
Medications are second line therapy and are tried first before proceeding to a permanent solution. If you have already failed medicines, we can proceed straight to an advanced treatment.
ADVANCED THERAPIES
Bladder Control Therapy delivered by the InterStim™ systems and advanced Botox® injections are two great options when conservative treatments don’t give you the relief you want. Read more below.
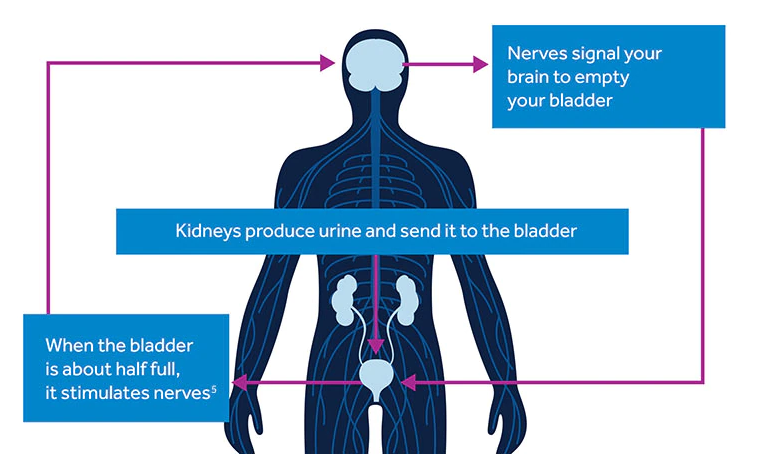
Medtronic Bladder Control Therapy Delivered by The InterStim™ System
Evidence suggests that breakdowns in the bladder-brain communication pathway are the root cause of OAB and non-obstructive urinary retention. While other therapies focus on the bladder muscles, Medtronic therapies target the nerves, which is thought to help restore normal bladder function. Medtronic bladder control therapy delivered by the InterStim™ systems provides life-changing relief. 84% of the patients who used the InterStim™ System was satisfied using it while 76% of people achieved success at 6 months compared to 49% who used medications.
When lifestyle changes and medications fail, Medtronic bladder control therapy delivered by the InterStim™ systems can help. This therapy is simple and discreet, and it delivers the kind of relief that lets you enjoy the activities you love without a second thought.
- Targets the nerves that control your bladder to help it function normally again
- 85% of people using the InterStim™ systems achieved success in the first year
- 3x greater improvements in quality of life compared to medications
- Lets you see if it works before you and your doctor decide
- Allows you to get full-body MRI scans if you need them
- More than 350,000 patients have experienced relief with this safe, FDA-approved and minimally invasive therapy
- Recharge-free and rechargeable options let you choose the right device for your lifestyle
The InterStim™ system offers recharge-free and rechareable options, so you can choose the right one for your lifestyle. The recharge-free InterStim X™ system may be best for most people as it’s convenient and low maintenance. The rechargeable InterStim™ Micro system is smaller and lasts longer, however, it requires regular recharging sessions.
InterStim X™ System

- Recharge-free battery
- Battery life: more than 10 years
- Device size: 12.5 cm cubed
- No routine maintenance
- SureScan™ MRI technology allows 1.5 and 3T full-body scans when certain conditions are met
InterStim™ Micro System

Rechargeable battery with Overdrive™ technology
- Battery life: 15 years
- Device size: 2.8 cm cubed
- Weekly recharging in approximately 20 minutes using a recharger, charging dock, and recharging belt
SureScan™ MRI technology allows 1.5 and 3T full-body scans when certain conditions are met
Is InterStim™ Right for You?
You may be a good candidate for Medtronic Bladder Control Therapy delivered by the InterStim™ systems if you have significant OAB symptoms or non-obstructive urinary retention, if you have tried lifestyle changes and oral medications, or if other therapies haven’t given you the relief you are looking for. Unlike other bladder control treatments, this therapy lets you try it first. It’s called an evaluation – like a test run, not a long-term commitment. We first start with a short, in-office procedure. You will be able to go about your regular activities for 3-14 days. During these days, we will help you track your symptoms to see if they improve and make a decision together if this is the right solution for you long-term. Take the next step by scheduling an appointment at one of our convenient locations!
OVERACTIVE BLADDER PATIENT TESTIMONIAL: OUR AMAZING RESULTS
A WINNING TEAM COMMITTED TO YOU
Are urge urinary incontinence, weak bladder control, and nighttime urination ruining your life? You are not alone. Our award winning team of bladder control experts will collaborate with you and provide the best best treatment for your bladder problems. The most important thing is that we know how to cure OAB and we are here for you.
BLADDER CONTROL SPECIALISTS
Advanced Urology LOCATIONS
OFFICE LOCATION
1557 Janmar Rd
Snellville, GA 30078
OFFICE LOCATION
10730 Medlock Bridge Rd
John’s Creek, GA 30097
OFFICE LOCATION
2695 Old Winder Hwy
Braselton, GA 30517
OFFICE LOCATION
2205 Riverstone Blvd Suite 101
Canton, GA 30114
OFFICE LOCATION
1371 Church Street Ext NW
Marietta, GA 30060
OFFICE LOCATION
1450 S Johnson Ferry Rd NE
Atlanta, GA 30319
OFFICE LOCATION
11660 Alpharetta Hwy
Roswell, GA 30076
OFFICE LOCATION
2711 Irvin Way
Decatur, GA 30030
OFFICE LOCATION
501 Crown Pointe Way
Lawrenceville, GA 30046
OFFICE LOCATION
1557 Janmar Rd
Snellville, GA 30078
OFFICE LOCATION
10730 Medlock Bridge Rd
John’s Creek, GA 30097
OFFICE LOCATION
2695 Old Winder Hwy
Braselton, GA 30517
OFFICE LOCATION
2205 Riverstone Blvd
Canton, GA 30114
OFFICE LOCATION
1371 Church Street Ext NW
Marietta, GA 30060
OFFICE LOCATION
1450 S Johnson Ferry Rd NE
Atlanta, GA 30319
OFFICE LOCATION
11660 Alpharetta Hwy
Roswell, GA 30076
OFFICE LOCATION
2711 Irvin Way
Decatur, GA 30030
OFFICE LOCATION
501 Crown Pointe Way
Lawrenceville, GA 30046